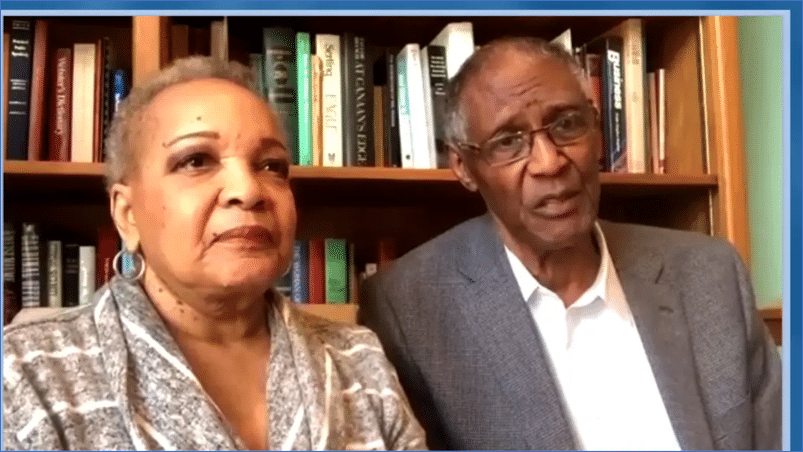
The Center for Clinical and Transitional Science and Training and Children’s Hospital brought together recognizable leaders in the Black community to say why they are motivated to get the COVID-19 vaccine.
Remember, all three vaccines available are 100% effective in preventing hospitalizations and deaths. It’s not the vaccine, It’s COVID-19 that’s the problem. Getting the vaccine means #GettingtoZero.
Courtesy of the Center for Clinical & Transitional Science and Training